Share this
Osteoporosis and Dental Implants
on September 15, 2015

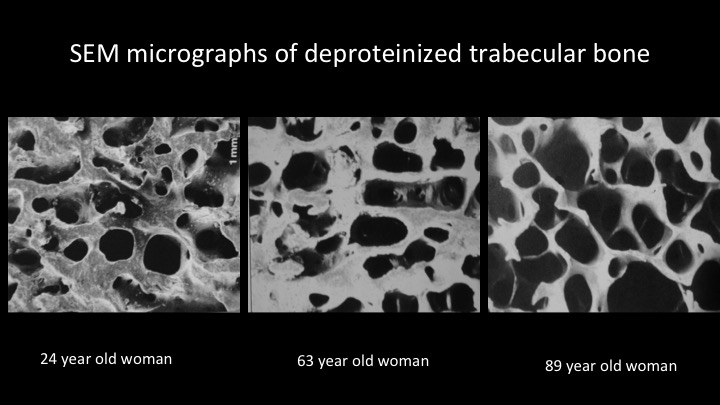
Osteoporosis is a condition whereby the bone is porous. This affects mainly older women who are post-menopausal although men are affected to a lesser extent as well. It is a fairly common condition and with an aging population, the incidence is set to rise. Osteoporosis weakens bones, making them easier to fracture. According to the Osteoporosis Society of Singapore, there are 402 cases of osteoporotic hip fractures per 100,000 population. Furthermore, a quarter of these do not survive the first year while another quarter becomes bedridden or wheelchair-bound. Many who needs dental implants are also in the elderly age group that may have osteoporosis. Does osteoporosis affect dental implant treatment outcome?
Dental implants are now arguably the best tooth replacement modality. It is the treatment of choice. However, unlike conventional crown and bridge, which is largely dependent of biomechanical properties of natural teeth to support a prosthetic tooth, implant-supported dental prosthesis involves a biological process of osseointegration, where the bone cells bond directly onto the surface of the implant. Being a biological process, it can be compromised by a variety of factors. In the case of an osteoporotic patient, the sparsity of the bone structure provides less bone cells as well as mineral scaffold to achieve good bonding between the bone and the implant. This in turn may affect the success of the implant both in the short term and long term.
However, in reality, it is not so straightforward, and fortunately so. Osteoporosis diagnosis is usually done by a test called dual x-ray absorptiometry (DXA) scan. This scan is done on the spine and hip as the main problem with osteoporosis concern these areas. When a DXA scan show a person to be osteoporotic, it means that the spine and hip bones are porous. However, DXA scans are not done routinely for the jaw bones. As such, someone diagnosed as osteoporotic by his physician or orthopedic surgeon may not have an osteoporotic jaw.
A study published in 2009 comparing DXA scans of the jaws and the hip showed no correlation between the two regions. This means that someone diagnosed with osteoporosis, typically with a DXA scan of the hip and spine, may not have osteoporosis of the jaw bones. The corollary to this is that an osteoporotic patient may not have a higher risk of implant failure compared with one who is not osteoporotic. Does this mean that we can ignore the results of DXA scans? Well, not quite. Each patient still need to be assessed individually.
DXA scans of the jaws are not routinely done and no calibration studies has been done yet on what range of values in bone mineral density constitute suboptimal level for dental implant placement. Currently, CT scans are often done primarily to assess bone shape and volume prior to implant placement. CT scans can provide a surrogate measure of bone density through the Hounsfield unit. The Hounsfield unit reference point is the density of water, which is given a value of zero, and air, with a value of -1000units. We can get a rough indication of bone density from the Hounsfield unit value of the part of the jaw that we can planning to insert the implant. However, this is by no means an accurate measurement as the value can vary according to the power and voltage of the x-rays machine as well as other factors peculiar to specific x-ray machines.
A good indication of the the density of the bone can be ascertained during insertion of the implant. A high insertion torque is indicative of good bone density and early restoration of the implant with a crown can be done safely. Conversely, a low insertion torque should be a warning to delay loading the implant.
While having osteoporosis does not preclude you from having dental implants, having had treatment for osteoporosis does have an impact. One of the more common types of drugs used to treat osteoporosis is bisphosphonates. Bisphosphonates are used to inhibit the action of the cells that resorbs bone, the osteoclasts. When the osteoclasts are prevented from "eating" up the bone, bone mass is preserved, hence arresting or slowing down the process of osteoporosis. These drugs can be given orally or intravenously, though the former is more commonly practiced. However, the collateral damage of bisphosphonates is that it also disturbs new bone formation as the old bone needs to be resorbed by the osteoclasts before new bone can be formed. Osseointegration of dental implants requires new bone to be formed and attached to the implant. When this process is disturbed, the implant cannot integrate. In some cases, not only does the implant fails, the bone also become infected because it is not able to repair itself adequately, resulting in greater breakdown of the bone. This a condition known as bisphosphonate-related osteonecrosis of the jaw (BRONJ).
Currently, there is no definite ways of treating BRONJ. Treatment is mainly targetting at minimizing infection and slowing the breakdown. Fortunately, the risk for most osteoporosis patients is not very high because the more common route of taking bisphosphonates is by mouth rather than intravenously. Current recommendations is to minimize or avoid surgery in the jaws for those who had intravenous bisphosphonates and that means no dental implants for this group. Those who are taking oral bisphosphonates have a lower risk but considering that dental implants are usually elective, it is best avoided as well.
Dental implants are highly predictable today with few contraindications. While osteoporosis is not a contraindication, having had bisphosphonates for treatment of osteoporosis does complicate any dental implant treatment outcome.
Share this
- Jaw Surgery (93)
- Dental Implants Singapore (90)
- Orthognathic Surgery (48)
- Replacing Missing Teeth (26)
- Missing Teeth Options (23)
- Underbite (23)
- Bone Grafting (21)
- Costs (18)
- Facial Aesthetics (18)
- Aesthetics (17)
- dental implants (16)
- corrective jaw surgery (15)
- BOTOX (11)
- Dermal Fillers (11)
- Wisdom teeth (10)
- Fixed Implant Dentures (8)
- Loose Dentures Singapore (6)
- Medisave (6)
- sleep apnea (6)
- Braces (5)
- Dental Pain (5)
- Dentures in Singapore (5)
- Loose Teeth (5)
- Tooth Extraction (5)
- jaw deformities (5)
- bimax (4)
- bone graft (4)
- maxillomandibular advancement (4)
- all-on-4 (3)
- bimaxillary protrusion (3)
- chin implant (3)
- facial asymmetry (3)
- full mouth dental implants (3)
- genioplasty (3)
- immediate implant (3)
- removal of an integrated dental implant (3)
- third molars (3)
- wisdom tooth surgery (3)
- My Dentures Don't Fit (2)
- VME (2)
- bone graft healing (2)
- distraction osteogenesis (2)
- medical tourism (2)
- obstructive sleep apnea (2)
- orthodontics (2)
- plastic surgery (2)
- CT guided dental implants (1)
- Double jaw surgery (1)
- Invisalign (1)
- Periodontal Disease (1)
- Permanent Dentures Singapore (1)
- before and after photos (1)
- facial trauma (1)
- fractured dental implant (1)
- oral appliance therapy (1)
- root canal treatment (1)
- veneers (1)
- vertical maxillary excess (1)
- September 2019 (2)
- July 2019 (2)
- May 2019 (2)
- August 2018 (1)
- October 2017 (1)
- September 2017 (2)
- August 2017 (1)
- June 2017 (2)
- May 2017 (4)
- April 2017 (1)
- March 2017 (1)
- February 2017 (3)
- January 2017 (3)
- December 2016 (1)
- November 2016 (2)
- October 2016 (4)
- September 2016 (9)
- August 2016 (5)
- July 2016 (11)
- June 2016 (14)
- May 2016 (6)
- April 2016 (2)
- March 2016 (1)
- January 2016 (7)
- December 2015 (10)
- November 2015 (4)
- October 2015 (9)
- September 2015 (7)
- August 2015 (1)
- July 2015 (6)
- June 2015 (3)
- May 2015 (7)
- April 2015 (5)
- March 2015 (8)
- January 2015 (5)
- December 2014 (7)
- November 2014 (7)
- October 2014 (6)
- September 2014 (8)
- August 2014 (5)
- July 2014 (7)
- June 2014 (8)
- May 2014 (9)
- April 2014 (10)
- March 2014 (6)
- February 2014 (8)
- January 2014 (3)
Subscribe by email
Email subscription




No Comments Yet
Let us know what you think